Suicide Touches the Lives of Many Vermonters.
If you or someone you know is thinking about suicide,
Call 988 for the 988 Suicide and Crisis Lifeline (formerly known as the National Suicide Prevention Lifeline) or text VT to 741741 for the Crisis Text Line. Trained counselors are available 24/7.
About the 988 Suicide and Crisis Lifeline in
American Sign Language (ASL) العربية (Arabic) Bosanski (Bosnian) မြန်မာစာ (Burmese) Chinese-Mandarin دری (Dari) English Français (French) Jamaican Patoois Kirundi (Ikirundi) Maay Maay नेपाली (Nepali) پښتو (Pashto) português (Portuguese) Soomaali (Somali) Español (Spanish) Kiswahili (Swahili) Kreyòl Ayisyen (Haitian Creole) Tigrinya (ትግርኛ) Українська (Ukrainian) Tiếng Việt (Vietnamese)
If you are concerned about your or a loved one's safety or need emergency medical services,
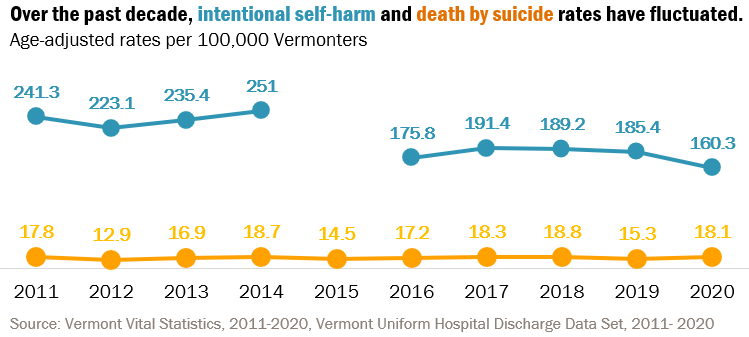
In 2021, there were 142 suicide deaths among Vermont residents. This is the highest number and rate of suicide deaths recorded in Vermont. Suicide impacts the whole community. Vermont’s intentional self-harm and death by suicide rates are significantly higher than the United States' rate. Suicide is also a major public health issue nationally.
Suicide is preventable and help is available.
Everyone has a role in saving lives and create healthy and strong individuals, families, and communities. Know the risk factors, recognize the warning signs and reach out to get help before and during a crisis.
FacingSuicideVT.com Initiative
Facing Suicide VT is a new statewide prevention initiative supported by the Vermont Department of Health and the Department of Mental Health through funding from the Centers for Disease Control and Prevention Comprehensive Suicide Prevention Program. This statewide prevention effort provides access to suicide prevention, education, support, and advocacy resources. By sharing our stories and talking about suicide in our state, we can make it easier to ask for help and get help when needed. We can help ourselves and each other when we start facing suicide in Vermont together. Learn more about Facing Suicide VT.
New Youth–Focused Resource: Suicide Prevention Trainings for Schools
The Vermont Department of Health and Department of Mental Health have developed a resource for school leaders and staff. This resource highlights the key elements of youth suicide prevention work in schools, as well as identifies free and low-cost trainings that are available in Vermont. This resource is one part of the state's comprehensive youth suicide prevention approach, which also includes providing community support and educational groups for youth at higher risk for suicide, training adults who work or care for youth to identify warning signs and connect youth to the appropriate care, supporting healthcare systems that treat youth having thoughts of suicide, and providing grief support groups for youth who have lost someone to suicide. This project is made possible through funding by the Substance Abuse and Mental Health Service Administration's Garrett Lee Smith Grant.