Multi-drug Resistant Organisms
Multi-drug resistant organisms (MDROs) are a growing public health concern in Vermont and across the country. These organisms can cause infections that are more difficult to treat leading to longer hospital stays, higher health care costs, and increased risk of severe outcomes.
According to the CDC, more than 2.8 million antibiotic resistant infections occur in the U.S. each year, and more than 35,000 people die from them. Read the report from CDC
Reportable in Vermont
Systematic, statewide surveillance for key MDROs is an essential part of controlling their spread. Confirmed and probable cases of the following organisms are reportable to the Vermont Department of Health. Click below for organism-specific information and resources.
CROs are Gram-negative bacteria that have developed resistance to carbapenems, a powerful class of antibiotics typically used to treat serious infections. They can cause pneumonia, urinary tract infections and bloodstream infections. CROs often live in the gut and spread through contact with contaminated surfaces or unwashed hands.
Patients and families (CDC) Health care providers (CDC)
CPOs are a type of CRO that produce an enzyme called carbapenemase, which breaks down carbapenem antibiotics. These antibiotics are often used as a last resort against severe infections. This type of resistance makes infections particularly difficult to treat and increases the risk of spread in healthcare settings. There are three main types of CPOs:
Carbapenemase-producing carbapenem-resistant Enterobacterales (CP-CRE)
Enterobacterales are commonly found in the human digestive tract. Many species of Enterobacterales are necessary for digestion and are usually harmless. However, these bacteria can cause serious infections when outside of the digestive tract.
Patients and families (Nebraska Health and Human Services) Health care providers (CDC)
Carbapenemase-producing carbapenem-resistant Pseudomonas aeruginosa (CP-CRPA)
Pseudomonas aeruginosa, can cause infections in humans including pneumonia, bloodstream infections, and surgical site infections. Some Pseudomonas aeruginosa bacteria are resistant to antibiotics.
Patients and families (CDC) Health care providers (CDC)
Carbapenemase-producing carbapenem-resistant Acinetobacter baumannii (CP-CRAB)

Acinetobacter baumannii is a key cause of healthcare-associated infections, CRAB bacteria can be very difficult to treat. CRAB can cause pneumonia, as well as wound, bloodstream, and urinary tract infections.
Patients and families (Washington Department of Health) Health care providers (CDC)

C. auris is an emerging, multidrug-resistant fungus that has caused outbreaks in healthcare facilities around the world. It can cause bloodstream and wound infections, especially in patients with invasive devices or prolonged hospital stays. C. auris is hard to identify with standard lab methods and is resistant to multiple antifungal medications.

iGAS is a rare but life-threatening infection caused by the bacterium Streptococcus pyogenes. It can lead to severe illnesses such as necrotizing fasciitis and toxic shock syndrome. These infections often require immediate medical attention and are more likely to occur in individuals with chronic illnesses, weakened immune systems, or skin lesions.
More information: Patients and families Health care providers (CDC)
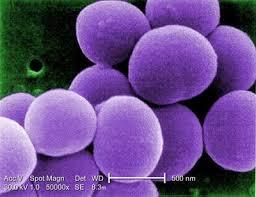
VRSA is a rare but serious strain of S. aureus that is resistant to vancomycin. These infections are particularly difficult to treat because they are resistant to nearly all available antibiotics. VRSA typically arises in individuals who are already colonized with both MRSA and VRE and who have received long-term antibiotic therapy.
Patients and families (CDC) Health care providers (CDC)
Not Reportable in Vermont
C. diff is a bacterium that causes severe diarrhea and colitis, often following antibiotic use. It produces spores that can survive on surfaces for long periods, making it highly transmissible in healthcare environments. C. diff infections can range from mild to life-threatening, particularly in older adults and patients with other illnesses.
Patients and families (CDC) Health care providers (CDC)
MRSA is a strain of S. aureus that is resistant to methicillin and related antibiotics. It is a common cause of skin infections, abscesses, and more serious conditions such as sepsis or pneumonia. MRSA is transmitted via direct contact, often through breaks in the skin or contaminated surfaces. It can be found in hospitals, nursing homes and in community settings.
Patients and families (CDC) Health care providers (CDC) MRSA in the Workplace (non-healthcare)
Enterococci are bacteria that live in the human gut but can cause infections if they spread to other parts of the body. VRE strains are resistant to vancomycin, an antibiotic typically used when other treatments fail. VRE can cause urinary tract infections, bloodstream infections, and surgical site infections, especially in patients with weakened immune systems.
Patients and families (CDC) Health care providers (Up to Date)
ESBL-producing bacteria, including some strains of E. coli and Klebsiella pneumoniae, are resistant to a wide range of beta-lactam antibiotics such as penicillins and cephalosporins. These organisms are a major cause of urinary tract infections and bloodstream infections, particularly in hospitalized or immunocompromised patients.
Patients and families (CDC) Health care providers (Up to Date)
What Health Care Providers Can Do
Healthcare workers and facilities play a critical role in preventing the spread of Multi-drug resistant organisms (MDROs). In addition to the steps below, there are also helpful resources available for treatment guidance and prevention protocols. Together, these tools support safer, more effective care across healthcare settings.
Key actions include:
- Follow infection prevention best practices. Use proper hand hygiene, wear protective equipment when needed, and disinfect shared equipment and surfaces between uses.
- Screen patients who may be at risk. Identify individuals who may be carrying resistant bacteria, especially those recently hospitalized or transferred from other facilities.
- Use antibiotics responsibly. Prescribe antibiotics only when needed, and choose the right drug, dose, and duration. This helps prevent resistance from developing.
- Isolate infected patients when necessary. Use contact precautions to prevent the spread to others, especially in hospitals and long-term care settings.
- Stay informed and report cases. Work with public health authorities to report resistant infections and follow guidelines on containment and control.




