Promoting Guidelines-based Care
Promoting and following guidelines-based care ensures that Vermonters with COPD are appropriately diagnosed and get the care they need.
The COPD National Action Plan is the first-ever blueprint for a multi-faceted, unified fight again COPD, providing guidance and information on building awareness, improving care, and turning policy to action.
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) Global Strategy for Prevention, Diagnosis and Management of COPD: 2025 Report outlines evidence-based strategies for COPD. A quick-reference guide is also available for physicians and nurses with key information about patient management and education.
The American Lung Association hosts an on-demand COPD Educator Course for respiratory therapists, internal medicine nurses, pulmonary nurses, pharmacists, and care managers.
COPD Prevention, Diagnosis and Treatment
Knowing who is at highest risk of developing COPD is a first step in providing prevention guidance and referrals. See the COPD: Chronic Obstructive Pulmonary Disease section to determine highest risk groups for COPD in Vermont.
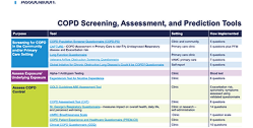
An early diagnosis is important to slow progression of COPD by getting patients on treatment and self-management plans and to avoid preventable emergencies. People who are at high risk of COPD and who also have early warning signs and symptoms (a lingering cough, difficulty breathing, fast worsening symptoms), should be screened for COPD. It is important that any prior diagnosis of COPD is confirmed by performing or seeing the results of spirometry or chest imaging.
Key action: Confirm a COPD diagnosis with a pulmonary function test (PFT), including evaluating with spirometry.
Spirometry remains the gold standard for diagnosing COPD.
Regularly scheduled follow-up care promotes stable COPD and reduces COPD-related emergencies. For patients at risk of exacerbation or for those who recently had a COPD-related emergency, more frequent follow-up care is essential for up to at least six months to ensure COPD is stabilized.